Cancer surgery
Our veterinarians’ high level of expertise and our practice’s fully equipped surgical suite allows us to perform the vast majority of soft tissue surgical procedures that your pet may require. Soft tissue surgery encompasses any surgery that is not related to bones. It includes procedures such as desexing, exploratory laporotomies, caesareans, lump removals, biopsies, wound stitch-ups, removal of intestinal foreign bodies — the list is endless!

A very common soft tissue surgery is the removal of lumps. Once they have been removed we often recommend sending them to our external laboratory for analysis.
Although most lumps are benign (not harmful), a minority are more serious (malignant). In the case of malignant (cancerous) tumours, early removal and an accurate diagnosis is extremely important to maximise the chances of a good outcome.
If you find a lump or bump on your pet please make an appointment to visit one of our veterinarians to discuss any surgery your pet may require.
Fundamentals of surgical oncology in small animals
Cancer is one of the major causes of morbidity in veterinary patients, and surgical removal of tumors one of the most common surgical procedures performed by veterinarians. This article covers tumor evaluation and biopsy, grading and staging, and surgical approach.
In human surgical oncology, 60% of human patients battling cancer are cured by surgery alone. Likewise, in veterinary medicine, surgery is considered the most important component of treatment in dogs and cats suffering from solid tumors because, in many cases, surgery offers the best chance for improving patients’ quality of life.
To help assure a positive outcome, the veterinarian needs a thorough understanding of the basic principles of surgical oncology, including:
• Characteristics of specific tumor being treated
• Surgical options available
• Potential need for adjunctive treatments, such as chemotherapy or radiation therapy.
Regardless of the treatment options sought, the overall goal of the therapeutic plan is to improve the patient’s quality of life.
Patient Evaluation
The patient’s treatment plan should be based on:
- Complete history
- Thorough physical examination
- Diagnostic imaging
- Clinical pathology with cytology
- Histopathology, when appropriate.
Tumor identification
The annual physical examination plays a key role in detecting neoplasia, either directly via palpation or through paraneoplastic syndromes, which may be found on routine blood and urine analysis. The physical examination allows detection of possible tumor presence and identification of concurrent conditions that may influence the treatment plan.
When a tumor is identified, record its size, location, and gross appearance, and palpate regional lymph nodes. If the lymph nodes are enlarged, firm, or immovable, the suspicion of a metastatic neoplasm rises; however, normal lymph node palpation does not guarantee lack of metastasis. Therefore, some form of lymph node biopsy is recommended in most cases.
Tumor evaluation
Histopathologic analysis of tissues obtained by biopsy allows definitive diagnosis of:
- Tumor type (hyperplasia, metaplasia, or neoplasia)
- Biological behavior (malignant or benign)
- Aggressiveness
- Tumor grade
There are 4 main types of tumor biopsy techniques
1. Fine-needle aspiration (FNA) is a cost-effective, minimally-invasive procedure that is useful for differentiating non-neoplastic from neoplastic diseases and, in many situations, obtaining a definitive diagnosis.
- FNA is usually reserved for cutaneous and subcutaneous masses; some tumors, such as mast cell tumors and lymphoma, are readily identifiable on most needle aspirates.
- Intracavitary structures (especially splenic and hepatic masses) may be sampled with ultrasonography or computed tomography guidance.
- However, FNA is generally the least diagnostic biopsy technique due to the minimal amount of tissue sampled and lack of organized tissue architecture, which prevents tumor grading.
- Certain tumor types, such as sarcomas, may not exfoliate cells well, leading to false-negative results. Interpret negative aspirates or aspirates with questionable results with caution, and utilize more aggressive biopsy techniques when clinically appropriate.
2. Needle-Core biopsy is more invasive than FNA but has proven to be highly diagnostic, with an accuracy of 100% for epithelial cell tumors and 94% for mesenchymal cell tumors. Needle-core biopsy includes 2 main techniques:
- Tru-cut needle-core biopsy (soft tissue)
- Jamshidi needle-core biopsy (ossified tissue).
- Typically, sedation and local anesthesia provide sufficient analgesia for biopsy collection. Caution should be used to avoid infiltrating anesthetic agents into the tumor to prevent distortion of the collected tissues
- Collecting multiple tissue samples increases the accuracy of biopsies.
3. Incisional biopsy is utilized when less invasive techniques fail to yield a diagnosis. Wedge and punch biopsies are examples of incisional biopsy techniques; they are:
- Especially useful for diagnosis of soft, friable, inflamed, and/or necrotic tumors.
- Commonly used to sample peripheral lymph nodes and masses located on the extremities.
- For most cases, include the border between normal healthy tissue and abnormal tissue, which allows the pathologist to determine extent of tumor invasion into normal tissue.
4. Excisional biopsy allows the identified tumor to be removed in its entirety, with or without additional surgical margins. While this is a common approach for mass removal in veterinary medicine, it remains controversial:
- It may provide a diagnosis and, therefore, a therapeutic plan, but the mass is removed without knowing the tumor type.
- It is also often impossible to excise the mass without contaminating clean tissue planes or complicating future surgical procedures.
- A less invasive biopsy procedure is generally recommended to guide the surgeon in choosing the appropriate method of surgical resection.
- Excisional biopsy is best reserved for cases in which adequate surgical margins are easily achievable with biopsy alone (eg, small cutaneous mass on trunk of a dog).
Biopsy procedure
Carefully plan the biopsy procedure to prevent spread of neoplastic cells to unaffected tissues and allow removal of biopsy tracks or scars during surgical excision of the tumor. When obtaining a biopsy from a vascular organ, such as the liver or spleen, coagulation testing should be considered. Although a presurgical biopsy is not always required, it is essential when the:
- Surgical plan will be affected by tumor characteristics.
- Tumor location will make closure of the surgical site difficult without reconstructive surgery (ie, skin flaps, grafts).
- Owner’s willingness to treat may be altered based on diagnosis.
- Once the biopsy is collected and properly preserved, have it processed and evaluated by a histopathologist.
Tumor grading
Tumor grade is the histopathologic assessment of the tumor’s aggressiveness, and includes information, such as the mitotic index, invasiveness into surrounding tissues, and degree of differentiation. This information is valuable when the surgeon is developing a treatment plan for the patient.
For some tumor types, the grading scheme may also include features, such as percent necrosis; for these neoplasms, a grade may not be accurately assessed by incisional biopsy.
Tumor staging
If the tumor is suspected to be malignant, tumor staging establishes to what extent the tumor has invaded local, regional, or distant (systemic) tissues.
Method of tumor metastasis is highly dependent upon the tumor type: Carcinomas and round cell tumors tend to spread via lymphatic routes, while sarcomas tend to spread via hematogenous routes. Common areas where metastatic disease is identified include the lungs and lymph nodes.
In most cases, the following diagnostics are recommended:
- Three-view thoracic radiographs
- Regional lymph node palpation
- Biopsy (as mentioned earlier, lymph node palpation does not guarantee lack of metastasis).
Additional diagnostics, such as abdominal ultrasound, may be needed depending on the biologic behavior of the tumor. Other modalities, such as computed tomography or magnetic resonance, may help increase the sensitivity of detecting metastatic disease and more accurately determine the local extent of the tumor in an effort to determine prognosis and help guide resection.
Surgical intervention
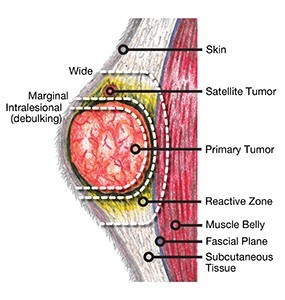
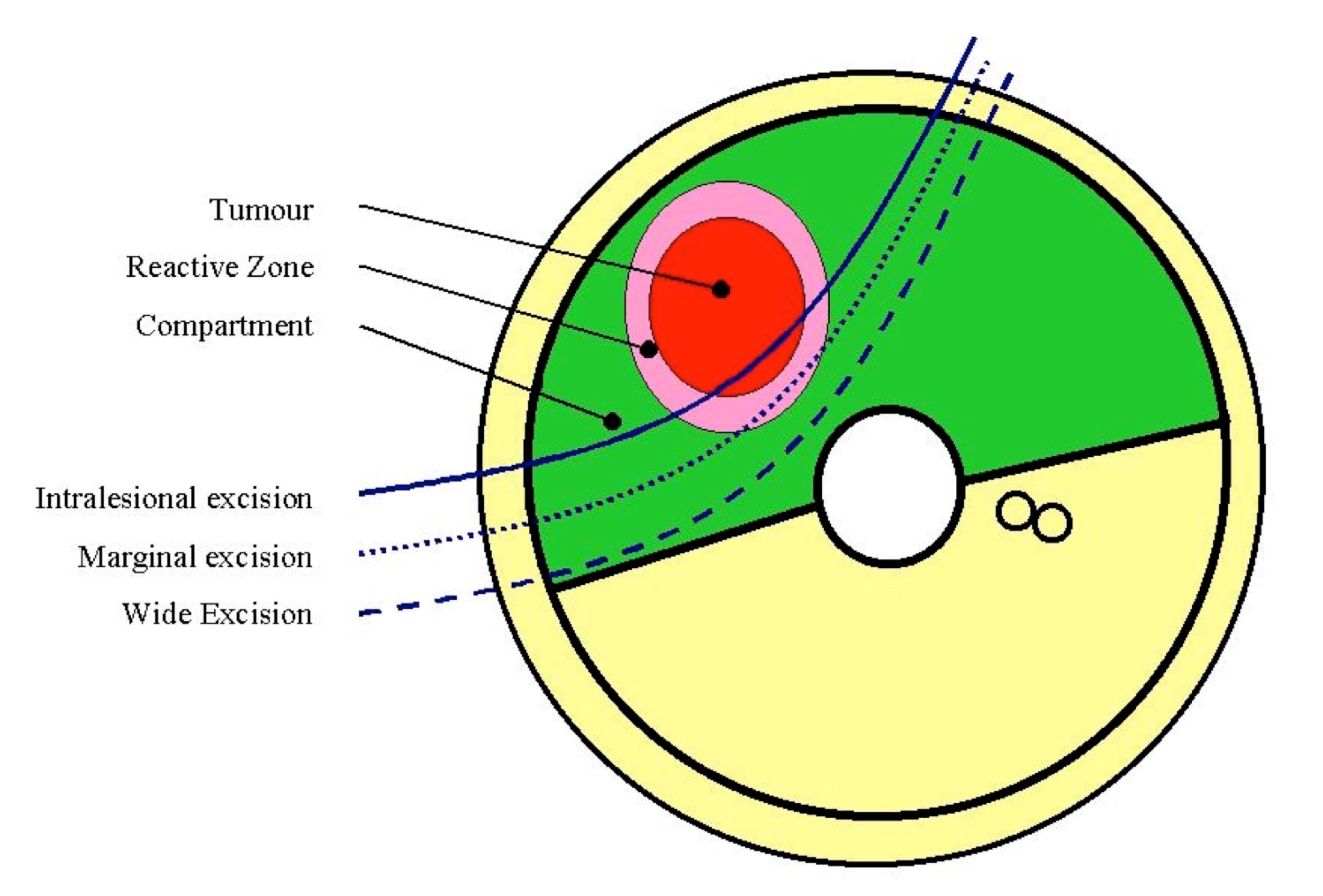
There are 4 levels of surgical aggressiveness, or surgical “dose,” to classify the extent of surgical resection. The most common surgical mistake is use of a surgical dose that is too low, which results from concerns about the ability to close the resultant defect. However, if the diagnosis of malignancy has been confirmed, it may be better to manage an open wound than leave tumor cells behind.

Surgical planning
Careful surgical planning should be performed, as the first surgery is often the surgeon’s best chance for achieving a positive outcome.
Multiple factors should be considered when determining aggressiveness of surgery:
- Type of tumor
- Short- and long-term prognosis
- Ability to achieve desired surgical margins, with an acceptable level of morbidity
- Concurrent disease
- Owner wishes
- Availability of adjunctive therapy, if needed following surgery.

